How you think about your depression has a profound impact on the experience of depression itself.
Specifically, when you have an overly-narrow and rigid way of thinking about depression, it often leads to more intense and longer lasting episodes.
For example, it’s not uncommon to hear people talk about depression like this:
- I’m depressed because my father was abusive
- If you just started thinking more positively, your depression would lift
- When I get depressed, I just can’t get motivated
- You’re depression comes from an imbalance of neurotransmitters in your brain
It’s not that these ideas are completely wrong….
- No doubt your father being abusive has something to do with why you’re depressed now
- And overly-negative thinking patterns absolutely do contribute to depression
The problem is that on their own, any one of these is rarely even close to being the whole story….
- Your father’s abuse may have triggered your first episode of depression when you were a teenager, but subsequent episodes could very likely have been triggered by other things like a difficult divorce or a lack of meaning in your work.
- Sure, an overly-negative thinking style isn’t helping your current depressive episode, but what’s driving that thinking style? Did you get unlucky and inherit the negative thinking gene or could it be that other factors in your life like your primary relationships, for example, influence how you tend to think about yourself and the world?
In my work as a therapist, one of the patterns I noticed among people who successfully worked through depression is that they started thinking much more flexibly and expansively about their depression.
Here are 5 things about depression most people don’t talk much about but are likely to help you think more carefully about depression, either your own or that of people you love.
1. Depression is not one thing
Depression is usually described as a disease or disorder, but it’s better thought of as a syndrome.
Diseases typically have a well-defined and understood symptoms and cause whereas syndromes are characterized by a collection of symptoms which often look very different from one person to another and frequently have different causal pathways.
When I worked as a therapist, it wasn’t uncommon to see three different clients struggling with depression in a single day, each of whom looked almost completely different from each other:
- John is a 66-year-old business owner who feels completely “empty” and “numb” inside and has for years. Although you would never know it because he has a great marriage, is wildly successful in his work, and had an incredible childhood. He’s charming, outgoing, and funny except for the rare moments when he opens up with me or his wife about how empty and numb he feels inside.
- Kaia is a 20-year-old college sophomore who feels “overwhelmingly sad” and can’t get out of bed most days. She overeats and ruminates almost constantly about what a “screw-up” she is.
- Danny is a 35-year-old who just became a father and is not coping well. He doesn’t mention feeling especially sad or unmotivated, but he notes being constantly tired, irritable, having trouble making decisions or even thinking straight sometimes. Occasionally, he has sudden bouts of suicidal thoughts that trigger spirals of anxiety and insomnia.
All three of these folks have the same diagnosis: major depressive disorder. And yet, they have wildly different histories, symptoms, and approaches to treatment. Isn’t it a little strange to say they’re all suffering from the same thing?
Understanding the huge variety of experiences that come with depression is important for a lot of reasons, many of which are common enough… For example, a lot of people discount their own symptoms because they don’t feel especially sad or suicidal. As a result, their depression goes untreated for a long time.
But there’s a less common though equally important reason to view depression as a multifaceted syndrome rather than narrowly defined disease…
Working through depression takes a lot of intellectual humility.
Many doctors and counselors aren’t very helpful with their depressed patients because they think they know the cause of their patient’s depression and they have the answer for how to treat it:
- Your serotonin levels are all off, that’s why you’re depressed. And that’s why you need to go on an antidepressant.
- You have unresolved trauma from your childhood and that’s the reason you’re depressed and need to spend an hour a week for years on end talking about how awful your parents were.
Obviously, brain chemistry and trauma, for example, can have profound effects on a person’s experience of depression. The problem is when people—either doctors or patients—get rigidly fixated on one idea of what their depression is or how to work through it.
Acknowledging and working through trauma, for instance, would of course be important for dealing with depression. But if it becomes the sole focus to the exclusion of thinking about other contributing factors—from cognitive styles and behavioral patterns to brain chemistry and diet—that’s dangerous.
Nobody likes the “it’s complicated” answer, but very often it’s the truth. And facing up to that with humility is usually a prerequisite for making real progress on depression.
So be very careful of people (yourself included) who claim to have the answer for the cause or cure of depression. And try to approach your depression with as much flexibility and humility as possible.
2. Compound depression
Many things can trigger depression initially. But one of the most common maintaining causes of depression is that people get judgmental with themselves for being depressed. Put another way, they get depressed about being depressed—something I call compound depression.
For example:
- Meg was a 32-year-old female and mother of three young children. After struggling with an initial bout of depression in college, she had been “depression free” for most of her 20s and early 30s.
- But then after the birth of her third child, she fell into another episode of depression that seems to have been triggered by a loss of meaning and struggle with her identity as a full-time mom and no longer working in her career.
- What was so striking about this episode of depression for Meg, though, was how much of it revolved around her depression. She was, in her own words, “thinking about depression constantly.”
- She spent a lot of time dwelling on her previous episode of depression and how she should have managed it better so that it wouldn’t have come back.
- She worried a lot that she would be “transmitting” her depression to her young kids and almost constantly criticized herself in her self-talk for not being “emotionally available” as a result of her depression (although there wasn’t much evidence that this was actually the case).
- Finally, she obsessed about her own inability to “shake off” her depression, attributing it to being weak and regularly telling herself that she “should be stronger for her kids.”
- Unsurprisingly, in addition to some of the classic symptoms of depression like loss of interest in normal activities and low energy, she was also experiencing many second-order symptoms related to being depressed about being depressed, primarily intense shame and guilt.
Meg’s story is a text-book example of compound depression. In particular, it highlights three of the most common mental habits that maintains compound depression:
- Rumination. Rumination is unhelpful negative thinking about the past. Specifically, it involves dwelling on past mistakes or failures well past the point of helpful reflection. It typically leads to a lot of guilt, shame, and regret.
- Self-criticism. Self-criticism is unhelpful negative thinking about the self, usually in the present. People who are especially stuck in the mental habit of self-criticism tend to use it as a default response to anything that goes poorly… Feeling lethargic in the morning → criticize self for staying up too late; kid misbehaving in school → criticize self for being a bad parent; been depressed for “too long” → criticize self for being weak willed. This habit of self-criticism leads to, among other things, a major loss of confidence, self-efficacy, and self-esteem.
- Worry. Worry is unhelpful negative thinking about the future. It often takes the form of catastrophizing and going to the worst-case scenario or imagining overly-negative ways in which other people are thinking about us. Worry can be an especially hard mental habit to break because it’s easy to rationalize as problem-solving. Unfortunately, worry with depression tends to keep people overly-sensitive and vigilant to negative information that reinforces their depression. And at the same time, it leads to ignoring or discounting potentially positive information or experiences that would be helpful.
Eventually, Meg did break free of her depression, but to do it, we had to work backward…
- Instead of focusing primarily on the thing that triggered this most recent episode (loss of meaning, role transitions, etc) we started by focusing on her overly critical self-talk and replacing it with more realistic and compassionate self-talk. This was challenging because, in her words, she didn’t “believe” it. But that was okay. As is often the case, belief and feeling are consequences of action, not prerequisites.
- Over time, her self-talk improved a bit. Not dramatically, but enough to take some of the pressure off her. As a result, she was able to focus a bit more on some of the identity issues that triggered the depression initially.
- As she made progress confronting and working through what it means to lose a part of her identity, she started noticing small changes to her energy levels. We took advantage of this to make small but steady improvements to her diet and exercise regimens which had seriously deteriorated during her depression. We also started doing some very small pleasure-mastery activities to begin building back a sense of agency and autonomy… She began working in her garden for 15 minutes a day, for example.
- Finally, as she took back more and more pieces of her life, she increasingly felt confident bringing other people back into her life. When she became depressed, Meg had—like so many depressed people—started avoiding other people and isolating herself. This was challenging because of all the shame she had experienced, but we worked very slowly and incrementally so that she had adequate time to build confidence that, despite what she had been telling herself, she had not “lost all my social skills.”
- It was a long journey, but eventually Meg did come out of her depression. The key point was that in order to have the space and energy to work on the initial causes of the depression she had to give herself some breathing room from the crushing self-criticism and judgment that came with her compound depression.
As we talked about in the introduction, how we think about depression has a profound impact on the experience of depression itself. In extreme cases, having an overly-negative and skewed view of your depression can lead to a kind of compound depression where we’re depressed about being depressed.
This distinction is especially important to be mindful of if you’re trying to live with or support someone else with depression. Because however insightful you think you are about what caused their depression (and therefore how they should work through it), it’s possible that the thing maintaining it is their attitude about their depression itself. Which means the most helpful thing to do initially might have nothing to do with the trigger of the depression and everything to do with helping them to be less judgmental and critical of themselves for being depressed.
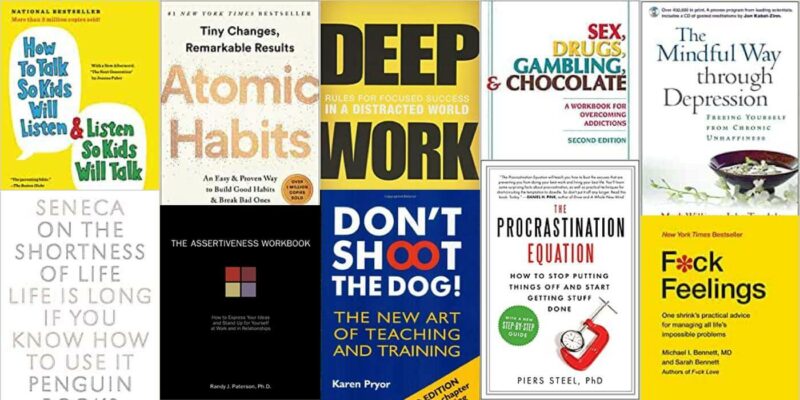
There’s an excellent book on this topic of depression about depression called the Mindful Way Through Depression which I did a short quote review of here if you’re interested →
3. The roads of depression are two-way streets
Here’s how we usually think of how medical diseases work:
Disease → symptoms
For example:
- Being infected with rhinovirus → runny nose
- Breaking your leg → pain and swelling
- A blocked artery → chest pain
And while this dynamic does happen, it’s simplistic to think that this is the whole story.
For example, in Type 2 diabetes, insulin dysregulation can lead to the symptom of increased appetite. But increased appetite can also lead to unhealthy eating which in turn can make insulin dysregulation worse.
The distinction between cause and effect—disease and symptom—is often not so simple.
For example:
- Is binge drinking a symptom or cause of alcoholism?
- Is high blood pressure a symptom or cause of heart disease?
The answer, of course, is both.
Diseases → Symptoms AND Symptoms → Disease
In many illnesses, the road between disease state and symptom is a two-way street. And very often the thing that caused an illness initially, is not the thing maintaining it.
I bring all this up to make the point that when it comes to depression, there’s rarely an easy answer to the question of cause and effect…
For example:
- Does depression cause low motivation? Or does low motivation make you depressed by cutting you off from energizing activities?
- Does being depressed make you sad? Or is sadness a trigger for negative-thinking patterns that make you depressed?
- Does depression cause you to isolate yourself and feel lonely? Or does loneliness and the tendency to isolate make you depressed?
- Does depression cause rumination and self-criticism? Or do self-criticism and rumination make you depressed?
- Do you drink because you’re depressed? Or are you depressed because you’ve spent half your life drinking?
Again, I’m not saying there’s an answer here. In fact, the whole point is that it’s complicated. And very often, both are true.
I’ve seen episodes of depression that were pretty clearly caused (or at least set in motion) by a habit of intense self-criticism and judgment. But I’ve also seen depression that’s triggered by a cocaine binge, which then had a lot of intense self-criticism as a symptom.
Here’s the big idea:
In depression, the relationship between cause and symptom is often a two-way street.
This is important to acknowledge because whether you successfully get through a period of depression often depends on addressing the right problems.
Unfortunately, many people with depression get fixated on the initial cause or trigger for their depression as the only thing that needs to be addressed (because, presumably, if it is then everything else will resolve itself).
For example:
- I had a client once who’s depression was undoubtedly triggered by a traumatic event and his traumatic response. But when he came to see me, he’d been depressed off and on for five years.
- As we worked together, it became pretty clear that the main factors maintaining his depression (and triggering new episodes) had little to do with the initial trauma. Specifically, he had developed a habit of isolating himself and severely restricting his activities anytime he made a significant mistake.
- In his mind, the trauma was the sole cause of his continued struggles with depression. And he was convinced that if he only processed his trauma correctly, all his other issues related to depression would take care of themselves.
- The problem was that there was no evidence that he hadn’t processed his trauma well. In fact, he actually seemed to have done a very good job of that initially and was not experiencing any of the usual symptoms of PTSD.
- But early on, someone had told him that “all depression is caused by unresolved trauma.” As a result, he’d been working valiantly for years to “resolve” his trauma with little positive impact on his depression. But also, he wasn’t addressing the things that were actually causing his depression now.
- Eventually, he began to let go of this fixation on trauma, and as a result, was able to start making significant progress on the other parts of his depression that were actually maintaining it.
To be clear, I’m not saying trauma can’t cause or trigger depression; I’m saying that in this case, it wasn’t the most relevant thing to focus on in terms of resolving the depression.
I’ve seen similar causes where people are convinced their negative self-talk is causing their depression, when in reality, they do have both PTSD and depression and treating the PTSD would be the best approach to eventually working through the depression.
The bigger point here is this:
Be flexible in how you think about cause and effect with depression.
Because very often what seems like a symptom is in fact the cause. And what was a cause may no longer be relevant.
If you or someone you know needs help working through depression, it’s important to consider working with a professional who will help you to think clearly and comprehensively about your depression.
Here are a few of my own thoughts on how to find a great a therapist →
4. Depression always happens in context
We human beings have become very good at manipulating our environments:
- We can cool our homes to 68 degrees with air conditioning despite it being 100 degrees outside
- We can listen to a podcast while shopping for groceries because of the amazing pocket supercomputers we have called mobile phones
- We can watch a movie or take a nap while flying hundreds of miles through the air in a jet airplane
But one of the side effects of this mastery over our environment is that—because we’re so good at manipulating our environments—we often forget how much environment still plays a role in our lives. And this is especially true when it comes to the impact our environment or context plays on our psychology.
A simple example:
- Often when I get stuck with a piece of writing, or find myself procrastinating on finishing an essay, I pack up my laptop in my backpack and head to the coffee shop down the street.
- I open my laptop, start writing, and almost always find that I can pretty easily get unstuck or quickly finish what seemed like a complete slog back home.
- In other words, a quick change of physical environment frequently reduces procrastination and writer’s block.
- So was I procrastinating because I didn’t have enough focus or willpower? Or was I procrastinating because, at that moment, my environment wasn’t very conducive to my work?
Here’s another example:
- I sometimes lose my temper with my kids in the evening before bed. But this happens much less frequently in the mornings. Why?
- One explanation is that my internal environment is very different. Specifically, by 7:00 pm I’m exhausted. And just like my kids, I have a much harder time regulating my emotions when I’m tired.
- So even though the external physical environment is the same, my ability to control my temper is greatly reduced when my internal physical environment (i.e. my body) is stressed and tired rather than relaxed and energized.
- So, when I reflect on why I lost my temper with my kids, my initial thought might be I lost my cool because I wasn’t patient enough. Which is true: I could have been more patient. But it’s also true that I lost my cool because my internal environment was stressed and tired, which makes it much harder to be patient.
Now, it shouldn’t be too hard to see how the same logic applies to our experience of depression…
Depression is highly contextual—influenced by the many environments in which it occurs.
We tend to think of depression as relatively context-independent…
- I’m depressed whether I’m at the office or in my bedroom
- I have depression at 65 same as when I was 25
- My depression makes me unmotivated whether it’s playing golf or gardening
And while it’s true that depression is not completely context dependent, it’s a mistake to swing all the way to the other extreme and assume that it’s the same regardless of context.
For example: In years of doing therapy with folks who struggled with depression, I can’t think of a single person who’s depression wasn’t at least modestly influenced by their social context. That is, certain relationships and communities tended to make it worse (being at home on the weekends with an unsupportive and argumentative spouse) while certain relationships seemed to help (talking with me in therapy or hanging out at a baseball game with a best friend).
This doesn’t mean that relationships are the sole cause/cure for depression. It just means that depression happens within social contexts. And those contexts frequently have a meaningful impact on the depression.
Here are a handful of other contexts that depression happens within:
- Neurochemistry. Depression happens within the context of your brain physiology. If you drink a bunch of alcohol and modify your neurochemistry temporarily, it will likely have an effect on your depression. Similarly, if you’ve been on antidepressants for 20 years, that will also impact your neurochemical context which will in turn affect your experience of depression.
- Work. Your work context often has a very large impact on your experience of depression. A highly stressful work environment, for example, can easily exacerbate your experience of depression. Similarly, having work that’s truly meaningful and that you love can have a profoundly positive influence on your depression.
- Weather. This might seem silly at first glance, but for many people, their geographic context and the weather they find themselves in on a regular basis can impact their experience of depression. People with seasonal affective disorder, for example, are significantly influenced by the amount of sunlight they are exposed to or not.
- Childhood. Your early experiences as a child can certainly impact your experience of depression. It’s well-known, for example, that childhood trauma significantly increases the risk for depressive episodes as an adult. On the other hand, having supportive caregivers and role models as a child can be a profoundly protective factor against depression as an adult. Your memories of childhood are a context.
- Behavioral Patterns. The behaviors you engage in on a regular basis, often without even thinking about them, are a context in which your depression happens. For example, if you’re in the habit of eating fast food on a regular basis, this can negatively affect your overall health and your microbiome which in turn can impact your experience of depression. Similarly, if you are in the habit of calling your best friend to chat every week on Friday afternoons, that might have a profoundly positive impact on your experience of depression (notice how different contexts overlap—in this case, the behavioral and social contexts).
- Mental Patterns. Your patterns of thought and belief are a context in which your depression lives. If your mind is full of self-critical and judgmental self-talk, for example, it’s not hard to see how that context would impact your depression.
- Values/Purpose. This one can be especially hard to notice, but all of us live within a context of values—things that are especially important and meaningful to us. And this values context can influence our experience of depression. For example: If you’re chronically sacrificing your values for someone else’s, that could absolutely impact your experience of depression. Similarly, doing work to clarify or update your personal values is often very helpful in working through depression.
The point of all this is to help you think more expansively about depression.
Many people stay stuck in depression because they only think about it in one or two contexts…
- They’re convinced their depression is the result of low serotonin levels in their brain and nothing else matters.
- They’re convinced that their depression is the result of overly negative self-talk and nothing but becoming more positive matters.
- They’re convinced that their depression is the result of childhood trauma and nothing but “resolving” that trauma can help their depression.
But in reality, depression happens within many, many contexts, all of which are likely to play a role—both in terms of how the depression started and is being maintained as well as how it can be resolved.
Everything from your genetics and temperament to your self-talk and sleep habits are likely to play a role in your depression. And if you want to understand and work through it effectively, it’s critical that you identify which contexts are most relevant to your experience of depression in this moment.
Consider this…
- You could try for decades to resolve depression by changing your brain chemistry. But if your depression is really being driven primarily by your lack of purpose and meaning in your career, you’re unlikely to find much success.
- You could do psychotherapy for years to analyze all the details of your difficult childhood and poor relationship with your parents. But if your depression is really being driven by an unhealthy relationship with your spouse, you’re unlikely to find such success.
- You could read every self-help book ever written about cultivating a positive mindset. But if your depression is really being driven by thyroid problems, you’re unlikely to find much success.
This is why it’s important to think broadly and carefully about the many contexts in which your depression occurs.
5. Depression is not a battle to be fought. It’s a message to be understood.
If you struggle with depression—or are trying to support someone who does—one of the best questions you can ask yourself is this:
What job is this depression doing?
At first blush, the idea that depression is doing a job might sound strange, but stick with me…
Here’s another question: Are fevers bad?
Well, having a fever is certainly uncomfortable… hot/cold flashes, muscle aches, fatigue, etc. And in rare cases an extraordinarily high fever can be dangerous and cause real damage to your body. But in any case, your fever isn’t trying to hurt you or make you feel uncomfortable. It’s a defense mechanism produced by your body that boosts your immune system and helps eliminate invading bacteria or viruses. In other words, a fever happens when your body knows you’re sick and wants to to help. It’s doing a job.
You can take a similar perspective on depression…
Despite it being painful, what if this depression is trying to help me somehow?
Like a fever, depression comes with all sorts of uncomfortable, even painful, side effects. But that doesn’t mean it’s not trying to help.
Let’s use some other common emotional struggles to explore this idea of depression doing a job…
- When you feel anxious, that’s your body trying to help you deal with a threat or danger. Most of the physical sensations we associate with anxiety—increased heart rate and respiration, sweating and temperature increase, muscle tension, etc—these are all the result of your brain releasing adrenaline which helps you to fight or flee something dangerous. Adrenaline is a performance enhancer that just happens to feel uncomfortable.
- When you feel guilty and keep replaying a mistake over and over again in your head, that’s your mind trying to make sure you don’t make a similar mistake in the future. Guilt can motivate healthy reflection.
- When you feel angry at someone, it motivates you to take action and correct an injustice.
Of course, these emotional reactions aren’t always helpful—frequently we get anxious when there’s no real threat or angry even though no one’s actually done anything wrong.
But that doesn’t change the fact that they’re still just trying to help. They’re doing a job. And when you realize this, it can profoundly change how you react to those difficult emotions…
- If you understand that your anxiety is just trying to keep you safe, you’re less likely to get anxious about being anxious, which is what leads to panic attacks.
- If you understand that your guilt is just trying to help you in the future, you’re less likely to criticize yourself for feeling guilty, which leads to feeling guilty about feeling guilty.
Seeing our emotional struggles as functional—doing a job—helps us to respond to them in a more empathetic and productive way.
And this is very often the case with depression.
Because depression has so many unpleasant effects—persistent sadness, lack of motivation, fatigue, even suicidal thinking—it’s natural to see it as an enemy to be eliminated.
The trouble is the more you think about your depression as an enemy the more it starts to feel that way:
- When your self-talk is full of statements like I hate this depression. It’s the worst! you’re training your brain to see depression as a bad thing—a danger or sign of weakness. Which means the next time you feel depressed, you’re going to feel bad about feeling bad (the compound depression we talked about in #2 above).
- The more you respond to your depression symptoms with avoidance or coping, the less confident you are going to feel getting on with your life despite feeling depressed (which often is one of the best ways to resolve depression).
Fighting with your depression only makes it worse.
But there’s another reason to stop viewing depression as an enemy to be defeated, and instead, as a friend who’s trying to help… It might have something helpful to say!
One way of looking at the question of what job depression is doing is to consider that it’s a messenger—your body’s way of saying you’re not getting something that you need.
To illustrate this, let me tell you a story about a former client of mine…
How Ramit learned to listen to his depression instead of running from it
I worked with a client once, we’ll call him Ramit, who came to see me because he’d been depressed off and on for years.
He had many of the classic symptoms of depression from low mood and lack of energy to oversleeping and chronically negative thoughts about himself and his worth.
We tried working on the depression from a few different angles: being less negative and more compassionate in his self-talk, behavioral activation around pleasure-mastery activities, increasing his socialization with friends, etc.
While these changes seemed to have a modest positive effect, his progress slowed after a few months and eventually he began to get more depressed because he felt hopeless that there was anything he could do to really change things.
At this point, I took a step back and tried to re-assess the approach…
- What were we missing?
- Clearly this depression was happening for a reason, we just hadn’t figured out why…
- What job was it doing?
- What was it trying to tell him?
To try and get better answers to these questions, I spent some time reviewing Ramit’s history and current life situation. And something that stood out was his job—specifically, how much he disliked not only his current job as radiologist but how disenchanted he was with the entire medical field.
He had spent decades of his life obsessed with the idea of becoming a doctor. But after years and years of training, he finally began working in the field only to realize how bad a fit it was for his personality and goals. And while he could acknowledge this dissatisfaction with his career, he couldn’t bring himself to really consider that he was in the wrong career—that he might be far happier and more fulfilled doing something completely different.
But slowly, as we spent more time talking about why he didn’t enjoy his work and the types of things he did love to do (he loved computers and actually coded his own software and apps in his free time) it became more and more clear that there was a HUGE mismatch between what he really enjoyed spending time working on (software and computers) and what he was telling himself he should spend his life doing (medicine).
Eventually, equipped with this new hypothesis about his depression—that it was a message about his need to be doing work that was personally meaningful and enjoyable to him—we started taking very small steps to explore how he might change careers…
- He put together a clear picture of his finances and savings and figured out how much runway he would have if he did want to make a change.
- He participated in a 14-day coding bootcamp to see how much he really enjoyed a more intense level of work in software.
- He set up some phone calls with friends of friends who worked in the software industry to hear their perspectives about it.
And sure enough, the more he started looking into and taking seriously this idea of a new career path, the more his depressive symptoms began to lift.
Eventually, Ramit made the leap… he left medicine and got a job as a software engineer for a startup. And while I haven’t heard from Ramit in years now, when we had our final session together he told me that not only was he glad that he was feeling so much less depressed, but for the first time since he was a kid, he was feeling really hopeful and excited about his future.
When it comes to depression, don’t shoot the messenger
Fighting or running away from depression usually ends up making it worse. But more importantly, it also causes you to miss what your mind is trying to tell you about what you need.
In Ramit’s case, his depression was a signal that there was a profound mismatch between what he was telling himself he wanted out of his career and work and what he actually wanted.
But the content of depressions’ message can be all sorts of things…
- Often depression is related to a lack of intimacy or depth in our core relationships.
- Depression can be a sign that our overall stress burden is far too high and unsustainable in the long-term.
- Depression can be fundamentally spiritual or existential in nature—a signal that, for example, we lack meaning or purpose in our lives.
Of course, I can’t say for certain that depression is always communicating some sort of message.
But if you’ve struggled with depression for a long time, and haven’t made headway with other approaches, it’s worth trying to think more functionally about depression and asking yourself:
What job is this depression doing? Is it trying to tell me something?
But remember, the message may not be something you want to hear…
- Changing careers
- Leaving a long-time partner
- Moving to a new city or country
- Updating your spiritual beliefs
These are all big, challenging, and potentially terrifying, options. So our instinct may well be to avoid them and discount them. But again, if you’ve struggled with depression for a long time, they’re worth giving some honest thought to.
All You Need to Know
Here are 5 things about depression most people don’t realize:
- Depression is not one thing
- Avoid compounding depression
- The roads of depression are two-way streets
- Depression always happens in context
- Depression is not a battle to be fought. It’s a message to be understood.
Learn More About Depression
Here are a few more articles of mine that you might find interesting:




16 Comments
Add YoursI’ve just read your article about 5 things about depression that most people don’t realise. At present my oldest son has moved back in with me after a traumatic split up with his wife. He is coping in many different ways, communication, sport, music and very often he tells me that he has an overwhelming desire to run away as fast as he can. I’ve spent hours walking and listening to him. He was diagnosed with Functional Neurological Disorder whilst in hospital after some very severe seizures. The psychologist told him that the break up had caused a trauma in his mind and each time he saw or spoke to his wife it would trigger it.
He is taking a mild antidepressent and is understanding his condition more.
From the article I can see that it’s not just the effect of the split but other factors in my son’s life which have creted his way of thinkng and feeling.
I am very interested in your articles and find it extrmely helpful not only for my family but for myself.
Kind regards
Jo
This article seems very helpful. Thank you very much!
nick, your no-nonsense approach to mental health is such a breath of fresh air in this complicated world. i look forward to reading your other thoughts on the topic of depression when they become available. thank you so much for the work you do to help us.
I’m in graduate school to become a clinical mental health counselor, and I want to be as well-rounded a clinician as possible. Your articles help. Thank you.
Hi Nick, I have a teenage stepdaughter with depression and I’m looking forward to sharing this with her when it’s complete. Alhtough I am a trained mental health first aider in the UK I have an issue with how depression is doshnosed and treated too and think an approch more like yours would benefit many. I have been influenced by Lost Connections – why you are depressed and how to find hope, by Johan Hari which is well worth a read.
Cheers
Anthony
have you ever covered the empath and the narcisstic relationship nightmare? How one can expediate their recovery and stand their ground to get some justice with these warped minded emotional children? and how about these people stuck in some time zone of when they were in their 20’s thinking they can still wear the same looks?????Talk about denial! Thank you for the insights! God Bless you!
This is excellent! True to my experiences with my own depressive episodes. Thank you for making information like this easily available to us.
This has been very insightful and informative.
It’s noteworthy in the last 30 years that the more we define, categorize, analyze and treat anxiety & depression, the worse it has gotten. Kind of a large scale version of rumination.
I often question this myself…
So informative! I love all your newsletters and this is my fav so far. We are all seeking answers and finding that one cause of depression to blame it on and nobody can explain it in reality.. thanks for voicing this out. Like every other ailment of human body medicine is only to manage the symptoms and not to find the cause or remove the problem. Thanks for your honest reviews everytime!
Thank you! Something just clicked for me re: your analogy that depression is a messenger to help vs. An enemy to fight. Thank you so much Nick
Dear Nick, this is a masterful and kind account; equipment for life. Thank you. M. ❤️
I think your articles very helpful sometimes
thank you this puts a different perspective on my depression. I have a lot of negative self talk even though I have been successful in life. I just feel like Im not good enough for my husband.
I wanna know more about this because this is really informative!